

Cleveland Clinic Melanoma Program Offers Expert |
|
||||||||
|
The concept of multidisciplinary care is gaining wide acceptance in many fields of medicine, particularly in cancer care. This is especially true in the management of cutaneous melanoma, where early diagnosis, accurate staging and appropriate surgical management can optimize the survival of patients. Advances in the understanding of melanoma biology underscore the need for a comprehensive approach to treatment involving dermatologists, pathologists, surgeons and medical oncologists. The Melanoma Program at Cleveland Clinic offers a multidisciplinary resource for community physicians that includes all of these subspecialties. The incidence of cutaneous malignant melanoma continues to increase. Epidemiologic data shows that a steady rise has occurred over the last three decades and it is estimated that the lifetime risk for developing a cutaneous melanoma is 1:75. The disease is largely seen in adults. Approximately 62,500 cases were diagnosed in the United States in 2008, and 8,400 deaths were attributable to metastatic disease.
A small subgroup of patients has a high risk for development of melanoma. These patients have an inherited/familial disorder known as Dysplastic Nevus Syndrome. They have multiple atypical/dysplastic nevi that transform into melanomas with relatively high frequency. They usually present with melanoma at a younger age. Synchronous and metachronous melanomas are more commonly seen in these kindred. These patients require careful lifelong follow-up. Prognostic Factors
The full thickness biopsy also allows evaluation of other important prognostic features including mitotic index, surface ulceration, the presence of tumor infiltrating lymphocytes, invasion of lymphatics or blood vessels by tumor cells, or invasion along nerve pathways by tumor cells (neurotropism). Melanoma StagingStaging of melnomas is a composite of the analysis of the primary tumor prognostic features, spread to local or regional lymph nodes, or spread to distant sites. Accurate staging requires a Sentinel Lymph Node Biopsy (SLNB) for all patients whose primary lesion has a Breslow’s depth greater than 1 mm, or higher risk features such as invasion of the reticular dermis, surface ulceration or a high mitotic index. SLNB should be done by an experienced surgeon prior to any wide-excision procedure. The SLNB technique can be particularly challenging in patients with melanomas of the scalp, face and neck. Following SLNB, an adequate wide excision is needed. Between 20 and 40 percent of patients with tumors 1 to 4 mm thick have node-positive disease. If the SLNB is positive, lymphadenectomy of the draining lymph node basin is indicated. These patients also are candidates for adjuvant therapy using alpha Interferon. Interferon is the only FDA approved treatment for Stage III (lymph node positive) disease and for patients with deep primary lesions (greater than 4 mms Breslow’s depth). For patients with Stage IV (metastatic) disease, the five-year survival rate is less than five percent. Chemotherapy does not reproducibly prolong survival, although some patients achieve significant disease regression. Patients also can do well if the disease is managed surgically by removing isolated metastases from skin (subcutaneous nodules), lung, liver and brain. Spontaneous regression of metastatic disease is well documented in the literature, suggesting that the immune system has a role in controlling the disease. While these remissions are uncommon, the observation has led to the use of Immunomodulating agents in the management of melanoma. Interleukin-2 in high doses has resulted in long-term remissions in a small subset of patients, at the cost of significant toxicity. Clinical trials are an important component of melanoma management. Most patients with Stage III and Stage IV disease are candidates for trial inclusion. Return to Current Issue |
|||||||||
Cleveland Clinic | Home | Agenda | Faculty


 Melanoma is a malignant tumor of melanocytes – cells derived from the neural crest – whose function is to produce melanin. While most melanomas arise in skin, they can manifest in mucosal surfaces or from other sites where neural crest cells migrate. While melanomas do arise from precursor lesions such as nevi, in more than 50 percent of patients, the melanoma arises in seemingly normal skin, without a precursor lesion. In women, melanoma occurs more commonly on the extremities and in men on the trunk, head and neck. Melanomas typically are pigmented lesions, but amelanotic melanomas do occur with some frequency, or may appear as a lesion with a pinkish hue. The histologic features of benign and malignant lesions can be very subtle and examination by an experienced pathologist (or more than one) is sometimes necessary to make an accurate diagnosis.
Melanoma is a malignant tumor of melanocytes – cells derived from the neural crest – whose function is to produce melanin. While most melanomas arise in skin, they can manifest in mucosal surfaces or from other sites where neural crest cells migrate. While melanomas do arise from precursor lesions such as nevi, in more than 50 percent of patients, the melanoma arises in seemingly normal skin, without a precursor lesion. In women, melanoma occurs more commonly on the extremities and in men on the trunk, head and neck. Melanomas typically are pigmented lesions, but amelanotic melanomas do occur with some frequency, or may appear as a lesion with a pinkish hue. The histologic features of benign and malignant lesions can be very subtle and examination by an experienced pathologist (or more than one) is sometimes necessary to make an accurate diagnosis. 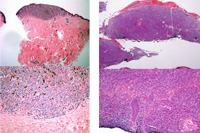 Several clinical and histological factors impact the prognosis in patients with melanoma. Thickness (Breslow’s depth) and level of invasion (Clark’s level) are of utmost importance. A full thickness punch biopsy of the skin down to the subcutaneous fat is the best way to determine the depth/level of invasion and shave biopsies are not appropriate for the evaluation of a melanoma. Cauterization of any pigmented lesion should be avoided.
Several clinical and histological factors impact the prognosis in patients with melanoma. Thickness (Breslow’s depth) and level of invasion (Clark’s level) are of utmost importance. A full thickness punch biopsy of the skin down to the subcutaneous fat is the best way to determine the depth/level of invasion and shave biopsies are not appropriate for the evaluation of a melanoma. Cauterization of any pigmented lesion should be avoided.